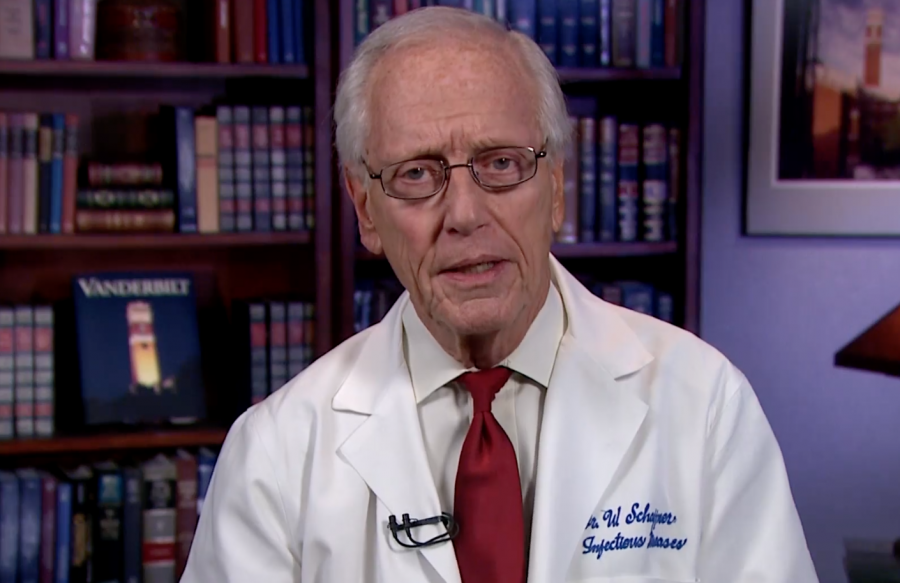
Professor of Medicine in the Division of Infectious Diseases William Schaffner spoke to The Hustler April 5 about the spread of the novel coronavirus. Schaffner is currently the Professor of Preventive Medicine in the Department of Health Policy. He graduated from Yale University in 1957, completed medical school at Cornell University in 1962, followed up with residency and his fellowship at Vanderbilt. Schaffner also served as the Epidemic Intelligence Service Officer with the Centers for Disease Control and Prevention (CDC) after his fellowship.
He is currently on the coronavirus advisory group for the National Collegiate Athletic Association (NCAA), which played a part in the cancelation of March Madness, and also works in a consulting role for PepsiCo. He is currently the Medical Director of the National Foundation for Infectious Diseases (NFID). In the past, he has been the President of the NFID and also a part of the Executive Board for the Infectious Diseases Society of America.
He currently is working on bridging the communication barrier between the general public and the medicinal community. He has been the face of coronavirus communications for Vanderbilt and hopes to inform the public about infectious diseases and other advancements in research.
COVID-19, belonging to the coronavirus family, originated in Wuhan, China Dec. 1 and has expanded to over 1.85 million cases globally. Countries with the most cases are, respectively, the United States, Spain, Italy, France and Germany. The United States currently has over 555,000 cases and 22,000 deaths. There is currently no publicly available vaccine for the coronavirus.
Vanderbilt Hustler: What has VUMC done in terms of logistics to stop the spread of COVID-19?
William Schaffner: The list is very long-ranging all the way from basic research to kind of what I do which is work with the media to get good messages out. The Medical Center has been in constant review of infection control practices and organizing our response so that we can take care of patients. And we’ve done this in collaboration with the Nashville Davidson County Metro health department and the state health department. The university itself has had several advisory committees that have worked with the university administration on various aspects of the impact of COVID-19 on the university itself.
What does COVID-19 currently look like in the state of Tennessee?
Currently, if you recognize that we are a large diverse country, the coronavirus is not at the same stage everywhere. There are obviously hotspots: New York City is right at the front line, but Detroit, New Orleans, Miami et cetera. We’re not there, but we are warming up. We’ve had an increasing number of COVID patients admitted to the medical center over the last several weeks. That number appears to be increasing weekly. So, I think we are approaching that time where we will hit our maximum in April and perhaps going into May.
One of the things that I’m involved with along with the state health department, we are part of a twelve-location research consortium sponsored by the CDC, and we are monitoring the population-based, laboratory-confirmed COVID admissions to hospitals in middle Tennessee—in Davidson and the surrounding counties. This is also what our colleagues are also doing around the country. We have seen in all parts of middle Tennessee in all these hospitals, in cases now being admitted that the increase is now speeding up over the last couple weeks.
How do we reintroduce people into society after social distancing? Wouldn’t a second wave be inevitable?
The answer is maybe. First of all, it’s obviously a complicated question, so there’s a bit of an elaborate answer.
At the moment, we have testing capacity; not as good as we would like by any means, but we have testing capacity to test for the virus. Fairly soon, within a matter of weeks to just the near term months, we’re going to have available another set of tests: they’re called antibody tests. They will be able to test the blood to see who’s had previous experience with the coronavirus and who has not. That will enable us in university settings, business settings and the like to begin to make some judgments about who we can expect to come back and is likely to be completely protected.
In the near term, over the next year or so, we don’t expect people to get second cases of this coronavirus. Then we can, as we open things up again, focus infection control to our susceptible colleagues. Obviously, we’re going to have to continue some elements of social distancing. The things that will open up last are large mass gatherings, concerts and things such as that. We may be asked, while opening up business, to still on a personal basis avoid large gatherings, birthdays parties, weddings and funerals until we’re convinced we can better manage whatever second wave appears.
One other thing is that we have a beautiful day today: it’s a wonderful, warm spring day. Is the new coronavirus seasonal, the way influenza is? As we know, influenza is strikingly seasonal; it goes away in the summer. I say it goes away, but if you were doing a research study, you could still find the occasional case of influenza. But for public health purposes, it basically goes away and comes back every winter. Will the coronavirus, which is also a respiratory virus, do something similar? I say similar because the human coronaviruses that cause common colds are seasonal, but they’re not as completely seasonal as influenza. So we anticipate that this coronavirus will diminish as the weather gets warmer, will smolder through the summer and may then come up again next winter sometime. By that time, many people in the population will have experienced the virus. I think the surge then will be much diminished.
Why would seasonality potentially impact the coronavirus as it does with influenza when there are still cases of coronavirus in warmer parts of the world?
It’s a little complicated. If you look hard for influenza in the tropics, countries closer to the equator, you will see that influenza is not very seasonal. It smolders along during all parts of the year, so it’s not as distinctively seasonal as it is in the temperate climates. So we’re in much more of a temperate zone, and that’s where influenza and other respiratory viruses have very distinct seasonal patterns. We don’t entirely understand what that is, but one of the elements may indeed be humidity.
It turns out in very humid air, the little microscopic droplets that we exhale, which could contain the virus, don’t hover in the air as long and fall more quickly to the earth. So that makes it more difficult for the virus to get from me to you in the summer than it does in the winter. I’m sure there’s science behind what I’ve just said, but we’re all rather convinced that’s not the whole story; we don’t know the whole story.
Are people who have previous experience with the SARS-1 virus better able to fight this one off?
We think that’s not the case. When we test the blood and the virus in the laboratory, people who have had SARS-1 do not seem to have protection against this virus. So, it’s strain specific.
How does being placed on a ventilator help a patient fight off the infection?
We know that this coronavirus can affect the lungs, and in doing so, it interferes with our ability to exchange gases. When that happens, you need a ventilator to help you breathe and help you with that gas exchange. That’s what we call supportive care. We’re doing this while the body itself is fighting off the virus. What we’re trying to do is maintain the body’s functionality while the body’s immune system fights off the virus. In effect, we’re trying to outlast the effect of the virus on the patient.
How many masks and ventilators does VUMC have?
I don’t know the exact number, but we have sufficient [numbers] in the near term. We’re being very rigorous about how they’re being used. We don’t let anyone use them for trivial reasons. We have done all kinds of exploration about our supply chain so that we can hope to have this supply, as we’re burning through it, replenished over time.
Is VUMC currently using the garage overflow space?
I think not yet. But I think we’re prepared to use it.
That was designed and constructed in absolutely record time. I was amazed when I walked through it. It was not yet completed the last time I was over there, but I was awed at how quickly that was designed and being constructed. The construction crews were absolutely working intensely when I had a chance to just look at it quickly a couple of weeks ago.

Are there plans to expand that space?
I think that’s the space that we’re capable of managing at the present time as an expansion. It takes not only space and all the accouterments in it along with all the beds and all the equipment, but it takes personnel. You can’t do it without personally taking care of the patients.
Does VUMC require its medical workers to take a test before they come back to work?
They have a process for doing that. Some of it involves testing and some it involves just getting better and waiting the appropriate amount of time according to the CDC guidelines. The CDC has guidelines that virtually all hospitals across the country are following in this regard.
Why did the CDC change its mask guidelines, from not suggesting community mask use to now recommending cloth-based masks be worn in all public settings?
The initial reasoning was not ‘it won’t work,’ it’s just that the scientific data to support that it will work was very thin. We didn’t have good data demonstrating there would be a good preventive effect if people out in the community wore masks.
Now, a major thing that has happened is not only that sick people transmit [virus particles] by coughing and sneezing, but you can be only mildly ill or not ill at all and transmit this virus. So, now the recommendation is not only stay home but when you have to go out, wear some facial protection that’ll provide some protection for you. Given that you might not know you’re infected, it will provide some protection for others also just in case you’re one of those asymptotic transmitters.
How is research being spread through the scientific community?
Just about everything you can possibly think of and then probably two dozen more things are under research somewhere. We have people at Vanderbilt working on a vaccine, drug treatments, convalescent antibody treatments and the creation of antibodies through monoclonal technology to treat people; all those are under investigation at Vanderbilt and elsewhere around the country.
Then, of course, people are doing a lot of clinical investigations trying to figure out why it is that people with certain underlying illnesses are apt to get the infection, people are looking at details of how the virus is getting spread in communities. All of those aspects are under investigation with people here and there. We have people at Vanderbilt looking at participating in these national research efforts in all aspects of coronavirus.
Robert Gottschalk contributed to the reporting of this article. The article has been edited for length and clarity.
Note: This article has been updated to reflect Dr. William Schaffner’s current role at the National Foundation for Infectious Diseases (NFID).