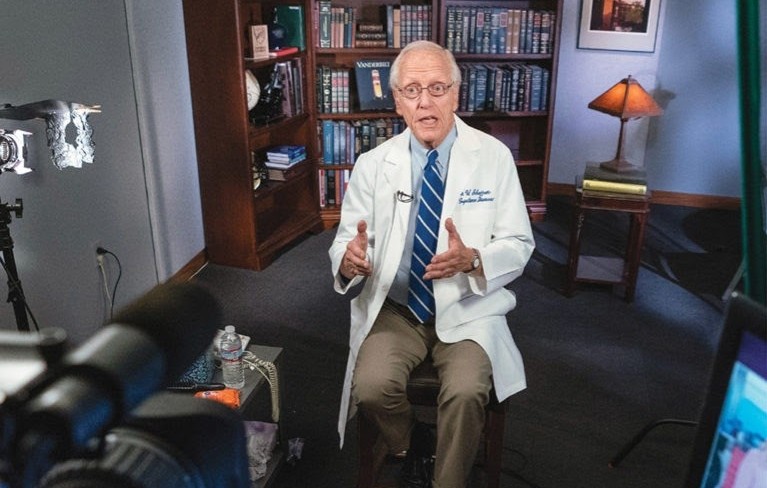
Dr. William Schaffner spoke to The Hustler on Aug. 25 to discuss COVID-19 updates and Vanderbilt’s return to campus. The Hustler last interviewed Schaffner on April 13, who spoke about VUMC research, pandemic severity in Tennessee and how to stay safe. Schaffner, Professor of Preventive Medicine in the Department of Health Policy as well as Professor of Medicine in the Division of Infectious Diseases at the Vanderbilt University School of Medicine, is the current Medical Director and past president of the National Foundation for Infectious Diseases (NFID). He has also served on the Executive Board for the Infectious Diseases Society of America.
Dr. Schaffner has been a spokesperson for Vanderbilt University in local and national media on communicable disease issues, translating research advances and public health events into language that the public can understand.
Vanderbilt Hustler: Where is the Nashville area currently in terms of pandemic severity and treatment capacity, and how has the state of affairs changed since April?
William Schaffner: Lots of things have happened since April. Things were doing well, and then they got worse because Nashville and the rest of the country opened up in a carefree way rather than in a careful way. So, cases went up, hospitalizations went up and deaths [as well].
The number of new cases is trending down in Nashville, not so much in the state, but certainly in Nashville. Hospitalizations and deaths, two indicators that are lagging, take longer to show any trends. [The rates] are remaining the same but (sic) are not getting worse. Also, the proportion of tests that turn out to be positive is actually down. That is a good indicator, so I am cautiously optimistic. We are just at the beginning of a trend that we would like to see continue. Wear the masks, social distance and avoid groups.
A recent study done by Duke has shown that certain types of face coverings such as neck gaiters or bandanas may actually be more harmful than wearing no masks at all. Can you corroborate these claims?
That’s been a widely cited study. We’ve always known that surgical masks and the face masks that have good, solid cloth are the best.
Bandanas are not good at all; they may be fashion-forward but are very ineffective. The issue of gaiters is actually not too surprising. For many of those materials, once you stretch them out over your nose or chin, you can almost see through them which would indicate that they are not very good. The idea that they may actually worsen things is a new idea. So, we should be cautious about that.
Is there evidence for the efficacy of wearing disposable gloves in a similar manner to face masks?
I think the data regarding gloves is much, much less clear. Hand hygiene is clearly important. Gloves can be misused. If you keep wearing gloves over a long period of time, they can become the same as your hands. Their utility out in the community, I think, is very limited. The emphasis ought to be really on hand hygiene: standard soap and water and hand hygiene gels.
Vanderbilt took a bold stance in choosing to bring students back on campus this fall. What major factors contributed to this decision?
Just speaking generally, I was one of the very several committees that were working on this. First, the committees first took a look at what was happening in our communities. It looked as though our community was getting better at handling COVID. Second, we have an excellent relationship with Vanderbilt University Medical Center (VUMC). We have worked very closely with the larger university community. Third, all of the committees that have been working on this have focused on student, faculty and staff safety.
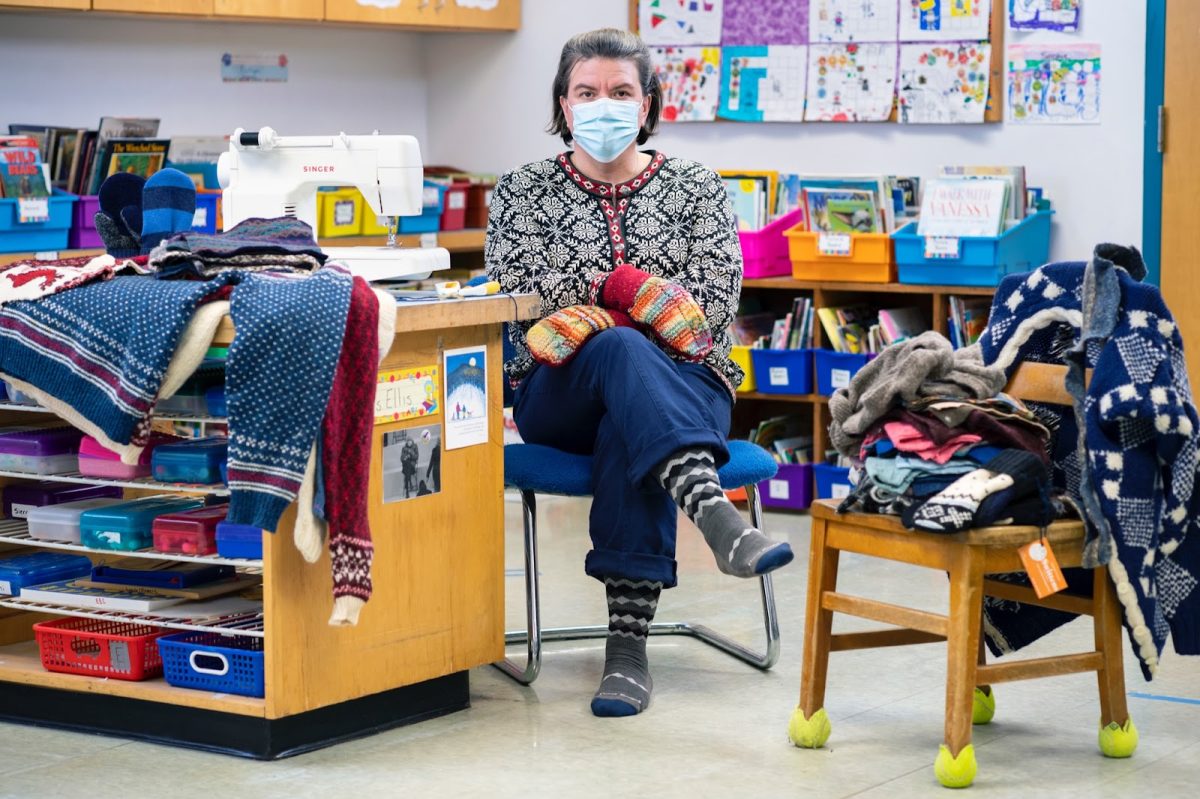
I want to tell you that every aspect of university life has been reviewed. Recommendations have been made, and there was a growing confidence that we can do this right. If students conform to social distancing regulations, we can make this work. We all, as faculty, staff and students, have this in our hands. If we’re careful, we can make it work. If we’re carefree, we’ll screw it up.
From a healthcare provider standpoint, can you speak to the detriments that a sustained lockdown would have/has had on Americans in regard to primary care?
It’s made a lot of people feel lonely and isolated. These are serious lockdowns that we are talking about. In terms of primary care, we’re now actually doing telehealth in ways we have never done before. We would have otherwise been very slow to move towards that. I think telehealth will continue to have a role going forward even after getting COVID under control. It’s important to remember that one thing you can’t do over telehealth is get vaccinated. In some adults and even among young children, vaccination rates are down. It is up to moms and dads to make sure that their and their children’s vaccinations are up to date.
All readers should be vaccinated against the flu this year. First of all, you’ll be protected, and we can try to ease the strain on the healthcare system. We know that we will likely have a flu outbreak. This is the best vaccine that science can produce for us today. We can reduce a lot of influenza, and even if you get the flu after you’ve had the vaccine—this can happen—you will have a much more mild infection. This is very important for people to realize.
Is there any evidence that you could be reinfected with COVID-19?
Only yesterday, it was in the news that a well-documented second infection was reported in the scientific literature. The second infection was documented by lab tests, but the individual did not have any illness. So, it appears that the person’s immune system was able to control the virus and not exhibit any symptoms. Nobody knows if this is a frequent phenomenon or not.
The world is waiting on a vaccine. What would the vaccine distribution plan look like, and do we have any semblance of a timeline at this point?
We’re actually a little optimistic that by the end of the year or the first quarter of the next year, one or more vaccines will become available. We all have to be “iffy” about this, because we have to see how the trials work. As you can imagine, on day one, we won’t have enough vaccines for 330 million people who live in the U.S. We have some vaccines available, but there won’t be enough. There will have to be a prioritization scheme. There are several national organizations working on this. I happen to be on one of them.
The first target will be healthcare workers for COVID patients. The second group is likely to be a larger group called “essential workers.” Who fits into that group is still yet to be determined. The next group would be vulnerable populations such as the elderly and those with underlying conditions, and after them, the general public. The distribution of the vaccine may be even more complicated than we think, because some of these vaccines must be administered in two doses over the course of a few months.
Do we know what the exact origin of the virus was at this point in time?
It is the overwhelming impression of the virologists of the world that this is indeed a virus that jumped species. It moved from an animal host to a human being on one occasion, probably, probably in a wet market in Wuhan, China. It did not originate in a Chinese research laboratory.
Has COVID-19 shown signs of mutation that we should be worried about?
The short answer is no. This has been a remarkably stable virus. It is not mutating to get more milder, get more severe or spread more rapidly. There are minor mutations such that the virology experts can trace the strains and say, “Oh, that one probably came from Europe, that one probably came from China.” But the basic viral structure has remained the same, and that bodes well for the development of vaccines because they will be right on target.
How is the COVID-19 outbreak different from or similar to previous viral outbreaks in recent history?
So, SARS and MERS also were coronaviruses that jumped species. All of these viruses are “cousins,” but they behave very differently. SARS and MERS were not as readily transmitted from person to person. It was harder to catch those viruses. That’s what we thought COVID was like in the beginning, but COVID showed us differently. Particularly, SARS infected much fewer people but made them sicker. COVID-19 is much more transmissible and thus, makes more people sick.
What does your day-to-day look like?
I spend a lot of my time organizing a public health consortium here. One of the tasks I’ve been given is actually to help track COVID infections. This is one of 12 locations around the country that are doing this. I’m also a member of any number of national committees that deal with public health so as you’d imagine, there are a lot of conference calls and Zoom meetings.
As you’ve observed, I’ve kind of become a national spokesperson for Vanderbilt and the national media.









Tom • Aug 2, 2023 at 8:24 am CDT
What are the side effects of the vax? What are the negatives of wearing face masks. Aren’t the viruses to small to be stopped by most masks. Is natural immunity better? Why should people continue to take an experimental vaccine if they have now obtained natural immunity? What is the actual ingredients of the vaccines? Why haven’t all the side effects of the vaccine been publicized – all drug commercials always list possible side effects, why don’t the people pushing the COVID vaccine list all side effects? Are they receiving money to say what they say from the drug companies? government agencies? Where are the opposing opinions about the safety and concerns of these shots? Can the vaccines produce covid variants even more lethal than the disease itself?